Systemic Lupus Erythematosus (SLE)
What is Systemic Lupus Erythematosus (SLE)?
Systemic Lupus Erythematosus (SLE), commonly known as lupus, is a chronic autoimmune disease that can affect multiple organs and systems in the body. It is characterized by periods of flare-ups and remission.
Who's at Risk for Systemic Lupus Erythematosus (SLE)?
SLE can develop in individuals of any age, gender, or ethnicity, but it predominantly affects women of childbearing age. It is more common in people of African, Asian, and Native American descent. Having a family history of lupus or certain genetic factors may also increase the risk.
What Causes Systemic Lupus Erythematosus (SLE)?
The exact cause of SLE is not fully understood, but it is believed to be a combination of genetic, environmental, and hormonal factors. Certain triggers, such as infections, medications, and exposure to ultraviolet light, may initiate or exacerbate the disease in genetically predisposed individuals.
How does Systemic Lupus Erythematosus (SLE) Start?
SLE often starts with nonspecific symptoms, making it challenging to diagnose in its early stages. The immune system mistakenly attacks the body's own healthy tissues, leading to inflammation and damage to various organs and systems.
What are the Symptoms of Systemic Lupus Erythematosus (SLE)?
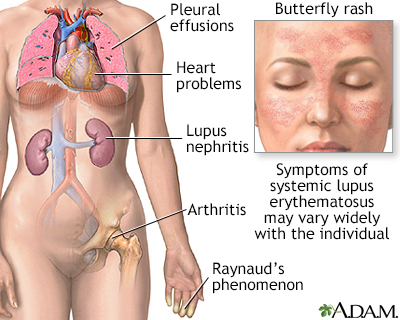
Symptoms of SLE can vary widely and may affect different parts of the body. Common symptoms include fatigue, joint pain and swelling, skin rashes (such as a butterfly-shaped rash on the face), sensitivity to sunlight, fever, hair loss, chest pain, and organ involvement, such as kidney or heart problems.
How is Systemic Lupus Erythematosus (SLE) Diagnosed?
Diagnosing SLE can be complex due to its varied symptoms and the absence of a definitive test. A healthcare provider will consider medical history, physical examination, blood tests to detect specific autoantibodies (such as antinuclear antibodies), and imaging or organ function tests to evaluate organ involvement.
How can Systemic Lupus Erythematosus (SLE) be Treated?
Treatment for SLE aims to manage symptoms, prevent flares, and minimize organ damage. This often involves a combination of medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, immunosuppressants, and antimalarial drugs. Lifestyle modifications, such as sun protection and regular exercise, are also important.
What Complications may Occur with Systemic Lupus Erythematosus (SLE)?
Complications of SLE can vary depending on the organs involved. These may include kidney damage, cardiovascular problems, lung inflammation, neurological disorders, blood disorders, increased susceptibility to infections, and complications during pregnancy.
How can I Prevent Systemic Lupus Erythematosus (SLE)?
As the exact cause of SLE is unknown, there are no specific preventive measures. However, managing known risk factors, such as maintaining a healthy lifestyle, avoiding excessive sun exposure, and seeking early medical attention for any concerning symptoms, can be beneficial.
Long-term Management of Systemic Lupus Erythematosus (SLE)
Long-term management of SLE involves regular medical follow-ups to monitor disease activity, adjusting medications as needed, managing symptoms, and making lifestyle modifications to support overall health. Emotional and psychological support is also important in coping with the chronic nature of the disease.
What is Recent Research Saying About Systemic Lupus Erythematosus (SLE)?
Recent research on SLE focuses on better understanding the underlying mechanisms of the disease, identifying new therapeutic targets, and developing more personalized treatment approaches. Researchers are studying genetic factors, immune system dysregulation, and environmental triggers to unravel the complex nature of SLE and improve treatment outcomes.
Where can I go for More Information on Systemic Lupus Erythematosus (SLE)?
For more information on Systemic Lupus Erythematosus (SLE), you can visit reputable sources such as the Lupus Foundation of America, the American College of Rheumatology, or the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Additionally, consulting with rheumatologists and healthcare professionals who specialize in autoimmune diseases can provide valuable insights and guidance.

