Tuberculosis
What is Tuberculosis?
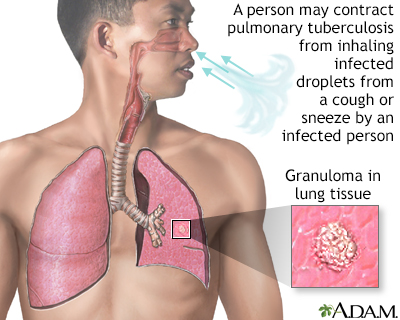
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also affect other parts of the body, such as the kidneys, spine, or brain. TB is transmitted through the air when an infected individual coughs, sneezes, or speaks, releasing droplets containing the bacteria. It is a significant global health concern, with millions of new cases reported each year. TB can be latent, where the bacteria remain dormant without causing symptoms, or active, where the bacteria multiply and cause symptoms.
Who's at risk for Tuberculosis?
Anyone can be at risk of developing TB, but certain factors increase the susceptibility to the infection. These include:
- Weakened immune system: Individuals with compromised immune systems, such as those living with HIV/AIDS or receiving immunosuppressive treatment, have a higher risk of developing TB.
- Close contact: Spending time in close proximity to someone with active TB increases the risk of transmission.
- Living conditions: Crowded living spaces, poor ventilation, and inadequate access to healthcare can contribute to the spread of TB.
- Travel to high-burden areas: Traveling to or residing in regions with a high prevalence of TB increases the risk of exposure to the bacteria.
What causes Tuberculosis?
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis. When an infected individual with active TB coughs, sneezes, or speaks, tiny droplets containing the bacteria are released into the air. Another person can become infected by inhaling these contaminated droplets. Once inside the body, the bacteria can travel to the lungs and invade the lung tissues. In some cases, the immune system is able to control the infection, leading to latent TB. However, if the immune response is inadequate, the bacteria can multiply and cause active TB.
How does Tuberculosis start?
Tuberculosis can start when an individual inhales the bacteria into the lungs. Once the bacteria enter the lung tissues, they can establish an infection. The immune system usually responds by activating immune cells to fight the bacteria. In most cases, the immune response is effective in controlling the infection, leading to latent TB. However, if the immune response is weakened or compromised, the bacteria can continue to multiply, causing active TB. Active TB is characterized by the presence of symptoms and the ability to transmit the infection to others.
What are the symptoms of Tuberculosis?
The symptoms of TB can vary depending on whether it is active or latent. Latent TB typically does not cause symptoms and is not contagious. However, individuals with latent TB have the potential to develop active TB in the future. Active TB can cause a range of symptoms, including:
- Persistent cough that lasts for more than three weeks.
- Chest pain or discomfort.
- Coughing up blood or phlegm.
- Fatigue or weakness.
- Unintentional weight loss.
- Loss of appetite.
- Fever and night sweats.
- Shortness of breath.
It's important to note that the symptoms of TB can be non-specific and may resemble those of other respiratory conditions, so a proper medical evaluation is necessary for an accurate diagnosis.
How is Tuberculosis diagnosed?
The diagnosis of TB involves several steps, including:
- Medical history and physical examination: A healthcare provider will inquire about symptoms, potential exposure to TB, and perform a physical examination to assess lung sounds and other signs.
- Tuberculin skin test (TST): Also known as the Mantoux test, a small amount of purified protein derivative (PPD) is injected into the skin. The reaction is assessed after 48-72 hours, and a positive result indicates exposure to TB but does not differentiate between latent and active infection.
- Interferon-gamma release assay (IGRA): A blood test that measures the immune response to TB proteins. Similar to the TST, a positive result indicates exposure but does not distinguish between latent and active infection.
- Chest X-ray or imaging: Imaging tests, such as a chest X-ray, can help evaluate the presence of lung abnormalities or signs of active TB.
- Sputum culture and microscopy: A sample of sputum (mucus coughed up from the lungs) is collected and analyzed to identify the presence of M. tuberculosis bacteria. This test confirms the diagnosis of active TB.
How can Tuberculosis be treated?
The treatment of TB involves a combination of antibiotics to eliminate the bacteria and prevent the development of drug resistance. The standard treatment regimen for active TB typically involves a combination of four antibiotics (isoniazid, rifampin, ethambutol, and pyrazinamide) taken for an extended period, usually six to nine months. It is essential to complete the entire course of treatment to ensure the eradication of the bacteria and minimize the risk of recurrence or the development of drug-resistant strains.
What complications may occur with Tuberculosis?
If left untreated or inadequately treated, TB can lead to various complications, including:
- Progressive lung damage: Active TB can cause progressive damage to the lung tissues, leading to lung scarring or cavities.
- Spread to other organs: The bacteria can spread from the lungs to other parts of the body, such as the kidneys, spine, or brain, causing localized infections or disseminated TB.
- Drug resistance: Inadequate or incomplete treatment can contribute to the development of drug-resistant TB, where the bacteria are resistant to standard antibiotics. Drug-resistant TB requires more prolonged and complex treatment regimens.
- Increased mortality: Without appropriate treatment, TB can be life-threatening, particularly in individuals with weakened immune systems or co-existing medical conditions.
How can I prevent Tuberculosis?
Preventing TB involves a combination of strategies, including:
- Vaccination: The Bacillus Calmette-Guérin (BCG) vaccine provides partial protection against severe forms of TB in children. However, it is not widely used in countries with low TB prevalence.
- Infection control measures: Proper ventilation, reduced crowding, and effective infection control practices in healthcare settings can help prevent the spread of TB.
- Timely diagnosis and treatment: Prompt identification and treatment of active TB cases can reduce the risk of transmission to others.
- Preventive therapy: Individuals with latent TB, particularly those at higher risk of progression to active TB, may benefit from preventive therapy with specific antibiotics to reduce the risk of developing active disease.
- Healthy lifestyle: Maintaining a healthy lifestyle, including regular exercise, a balanced diet, and adequate rest, can help boost the immune system and reduce the risk of developing active TB.
Long-term management of Tuberculosis
Long-term management of TB involves monitoring for treatment response, adherence to medication regimens, and follow-up care. Individuals receiving treatment for active TB need regular medical evaluations, including clinical assessments, monitoring for side effects, and periodic sputum tests to ensure the effectiveness of the treatment. Supportive care, including nutritional support and counseling, may be beneficial for individuals recovering from TB. Education about infection control measures and the importance of completing treatment is essential to prevent recurrence and the development of drug-resistant strains.
What is recent research saying about Tuberculosis?
Recent research on TB has focused on improving diagnostic techniques, developing new treatment regimens, and addressing drug resistance. Advances in molecular diagnostics, such as nucleic acid amplification tests (NAATs), have improved the accuracy and speed of TB diagnosis. Researchers are also investigating the use of new drugs and drug combinations, including shorter treatment regimens, to improve treatment outcomes and reduce the duration of therapy. Efforts to understand the genetic factors associated with drug resistance and develop new drugs targeting resistant strains are ongoing.
Where can I go for more information on Tuberculosis?
For more information on TB, reliable sources such as the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), or reputable tuberculosis organizations and healthcare institutions can provide valuable information and resources. These organizations offer comprehensive information on TB, including prevention strategies, treatment guidelines, global TB statistics, and ongoing research updates. Consulting with a healthcare professional, such as an infectious disease specialist or pulmonologist, can also provide personalized information and guidance specific to an individual's situation.

