Gastroesophageal Reflux Disease (GERD)
What is gastroesophageal reflux disease (GERD)?
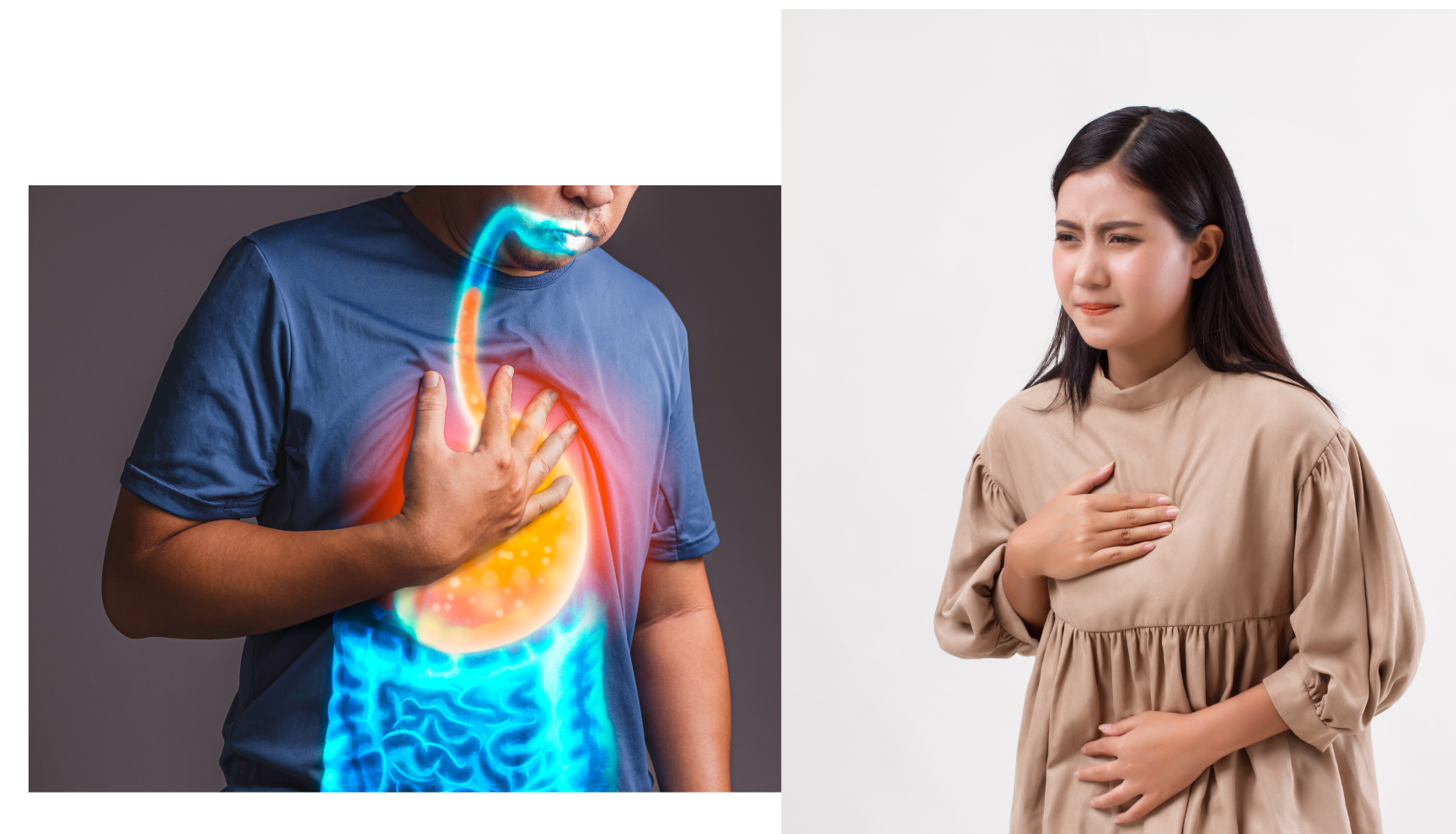
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder that occurs when stomach acid or bile flows back into the esophagus, the tube that connects the mouth to the stomach. GERD can cause a range of symptoms and may lead to complications such as esophagitis or Barrett's esophagus.
Who's at risk for GERD?
Anyone can develop GERD, but certain groups of people are at higher risk, including:
- People who are overweight or obese
- People who smoke or use tobacco products
- Pregnant women
- People with a family history of GERD
- People with certain medical conditions, such as hiatal hernia or scleroderma
What causes GERD?
GERD can be caused by various factors, including:
- Weak or dysfunctional lower esophageal sphincter (LES), the muscle that separates the esophagus from the stomach and helps prevent reflux of stomach contents
- Hiatal hernia, a condition in which part of the stomach pushes up into the chest through the diaphragm
- Delayed stomach emptying, which can increase the risk of reflux
- Lifestyle factors, such as diet or alcohol consumption, which can trigger or worsen reflux symptoms
How does GERD start?
GERD typically starts as a result of repeated or chronic exposure to stomach acid or bile in the esophagus. The condition may start gradually and worsen over time, or it may be triggered by specific factors such as certain foods or medications.
What are the symptoms of GERD?
The symptoms of GERD may vary depending on the severity and duration of the condition, but may include:
- Heartburn or acid reflux, a burning sensation in the chest or throat
- Regurgitation of food or stomach contents
- Nausea or vomiting
- Difficulty swallowing or a sensation of food getting stuck in the throat
- Chest pain
- Chronic cough or sore throat
How is GERD diagnosed?
Diagnosing GERD involves a comprehensive evaluation of a person's symptoms, medical history, and physical exam, as well as diagnostic tests such as an endoscopy or pH monitoring to confirm the presence and severity of reflux.
Let's look at more detailed information about ways GERD can be diagnosed:
Gastroesophageal reflux disease (GERD) is diagnosed based on a combination of clinical symptoms, the patient's history, and, when needed, specific diagnostic tests. Here's how the diagnostic process typically unfolds:
-
Clinical History and Physical Examination: Most often, the diagnosis starts with the doctor taking a detailed history of the patient's symptoms. Common symptoms include heartburn (a burning sensation in the chest), regurgitation of acid or food into the mouth, and occasionally, difficulty swallowing. If these symptoms are typical and respond to treatment, further diagnostic tests might not be necessary. When you see or speak with a doctor or health professional, it is helpful if you can write down a list of your symptoms so your doctor can get the most accurate clinical history when speaking with you.
-
Response to Proton Pump Inhibitors (PPIs): Sometimes, doctors might recommend a trial of proton pump inhibitors (a class of medication that reduces stomach acid production) to see if the patient's symptoms improve. A positive response can support the diagnosis of GERD. Some of these medications may be obtained over the counter or by prescription. It's very important you speak with your doctor before taking PPIs so you fully understand the risks and benefits of these medications.
-
Upper Endoscopy (Esophagogastroduodenoscopy or EGD): An endoscope is a thin, flexible tube with a camera on its tip. During this procedure, the doctor inserts the endoscope through the mouth to examine the esophagus, stomach, and the beginning of the small intestine. This test can reveal inflammation, ulcers, or other abnormalities that might be due to GERD. It's particularly used for people with chronic symptoms, those with additional concerns like difficulty swallowing, or if Barrett's esophagus (a pre-cancerous change) is suspected.
-
Esophageal pH Monitoring: This test measures the acidity inside the esophagus. It can confirm the presence of acid reflux and help to correlate reflux episodes with symptoms. The patient may wear a probe for 24 hours that measures pH levels, or a small capsule might be attached to the esophagus during an endoscopy, which transmits pH data wirelessly.
-
Esophageal Manometry: This test measures the pressure and movement of the esophagus, particularly evaluating the function of the lower esophageal sphincter (the muscular ring between the esophagus and the stomach). It can help determine if there are motility problems contributing to GERD or other conditions like achalasia.
-
Barium Swallow Radiograph: This is an X-ray test in which the patient swallows a liquid containing barium. The barium coats the inside lining of the esophagus and appears white on an X-ray, allowing the physician to see the shape and function of the esophagus. This test can reveal hiatal hernias, strictures, or other structural abnormalities.
-
Bile Reflux Testing: Since bile reflux can also cause symptoms similar to acid reflux, specific tests can be done to identify the presence of bile in the stomach or esophagus.
If GERD is suspected based on clinical history, often, the doctor might first recommend lifestyle modifications and medications before resorting to diagnostic tests. Testing is more common if there are atypical symptoms, the diagnosis is uncertain, or if complications are suspected. Always consult with a gastroenterologist or primary care physician if you believe you have GERD or any other gastrointestinal condition.
How can GERD be treated?
Treatment for GERD may involve a range of interventions, including:
- Lifestyle changes, such as avoiding trigger foods or losing weight, may help reduce reflux symptoms
- Medications, such as proton pump inhibitors or H2 blockers, can help reduce the amount of acid produced by the stomach
- Surgery, such as fundoplication, which involves tightening the LES and reducing the risk of reflux
What complications may occur with GERD?
If left untreated or poorly managed, GERD can lead to a range of complications, including:
- Esophagitis, inflammation or damage to the lining of the esophagus
- Barrett's esophagus, a condition in which the cells of the esophagus change and increase the risk of developing esophageal cancer
- Stricture or narrowing of the esophagus, which can make swallowing difficult or painful
How can I prevent GERD?
Preventing GERD involves a range of strategies, including:
- Maintaining a healthy weight and avoiding rapid weight gain. Weight gain around the abdomen can increase the risk of GERD.
- Large meals can bring on GERD because large meals stretch the stomach and increase your risk of acid reflux back up into your esophagus. So, one thing to try is eating smaller meals and then increasing the number of small meals you take in.
- Eating a balanced diet that is low in acidic or spicy foods.
- Walking after a meal may also aid in digestion and help reduce the symptoms of heartburn or acid reflux.
- Along with watching those foods you take in, reducing or eliminating alcohol consumption is a great way to reduce your risk of GERD.
- Quitting smoking is key because smoking can weaken the lower esophageal sphincter muscle and make it easier for acid to reflux back up into your esophagus.
- Elevating the head of the bed 6 to 8 inches can help (use a wedge pillow)
- Avoid lying down for at least 3 hours after meals. This is especially true at night. Plan your evening meals so you can have at least 3 hours before you will sleep.
Herbal remedies that have been explored to reduce or prevent symptoms of GERD include the following:
-
Licorice (DGL): Deglycyrrhizinated licorice (DGL) has been used to soothe inflammation in the stomach and may help with symptoms of GERD. Make sure to choose DGL and not regular licorice, as excessive amounts of the latter can lead to hypertension and other side effects.
-
Slippery Elm: Slippery elm bark has been used historically for various ailments, including GERD symptoms. It's believed to coat and soothe the stomach and esophagus.
-
Marshmallow root: Similar to slippery elm, marshmallow root can provide a soothing effect on the esophagus and stomach lining.
-
Aloe Vera juice: Some people drink aloe vera juice to relieve GERD symptoms. However, it's essential to ensure the juice is free of latex, which can cause diarrhea.
-
Chamomile: Chamomile has anti-inflammatory properties and may help to reduce the inflammation associated with GERD. Drinking chamomile tea before bedtime might help in reducing nighttime symptoms.
-
Ginger: Often used to treat nausea, ginger can also help reduce stomach acid and act as an anti-inflammatory. You can consume it as tea or add it to foods.
-
Turmeric: This spice has been studied for its anti-inflammatory properties and can potentially reduce inflammation in the esophagus and stomach.
As with all treatments, make sure you speak with a knowledgeable healthcare provider to make sure there are no known interactions between an herbal remedy you are considering and any prescription medication you are taking.
Long-term management of GERD
Managing GERD over the long term involves ongoing monitoring of symptoms, regular healthcare provider visits, and following a treatment plan as prescribed by a healthcare provider. It may also involve making lifestyle changes to manage symptoms and prevent complications.
What is recent research saying about GERD?
Recent research in GERD has focused on improving the diagnosis and management of the condition, as well as identifying new treatment options and risk factors. Some of the promising areas of research include:
- Investigation of the role of the gut microbiome in GERD, which may lead to new approaches to prevention and treatment.
- Development of new medications or drug combinations, which may be more effective at reducing acid production or improving LES function than current treatments.
- Exploration of the association between GERD and other medical conditions, such as asthma or sleep apnea, which may help identify high-risk groups and improve management strategies.
- More controlled trials are also needed to investigate the safety and efficacy of the herbal treatments noted above.
Where can I go for more information on GERD?
If you or someone you know has been diagnosed with GERD or wants more information on how to prevent the condition, it is important to seek help from a healthcare provider who specializes in the treatment of digestive disorders. The following organizations also provide information and resources on GERD:

