Inflammatory Bowel Disease
What is Inflammatory Bowel Disease?
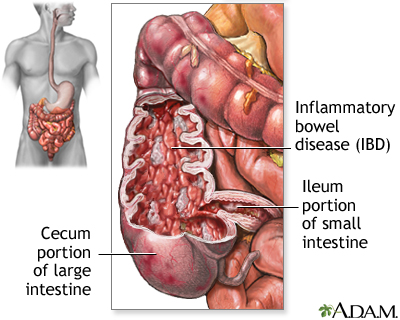
Inflammatory bowel disease (IBD) is a term used to describe a group of chronic inflammatory conditions that affect the gastrointestinal (GI) tract. The two main types of IBD are Crohn's disease, which can affect any part of the GI tract, and ulcerative colitis, which primarily affects the colon and rectum. IBD can cause a range of symptoms and complications that can significantly impact a person's quality of life.
Who's at risk for Inflammatory Bowel Disease?
IBD can affect people of all ages but is most commonly diagnosed in individuals between the ages of 15 and 35. Risk factors for IBD include a family history of the disease, being of Ashkenazi Jewish descent, smoking (particularly for Crohn's disease), and living in an industrialized country or urban area. Some studies also suggest that a diet high in processed foods and low in fruits and vegetables may increase the risk of developing IBD.
What causes Inflammatory Bowel Disease?
The exact cause of IBD is not well understood, but it is believed to involve a combination of genetic, environmental, and immune system factors. In individuals with IBD, the immune system mistakenly attacks the cells of the GI tract, leading to inflammation and damage.
How does Inflammatory Bowel Disease start?
IBD begins when the immune system starts to attack the cells of the gastrointestinal tract, leading to chronic inflammation and damage. This immune response may be triggered by a combination of genetic, environmental, and microbial factors, although the exact cause remains unclear.
What are the symptoms of Inflammatory Bowel Disease?
Symptoms of IBD can vary depending on the specific type and severity of the disease. Common symptoms include abdominal pain, diarrhea (sometimes with blood), weight loss, fatigue, and fever. The severity and frequency of symptoms can fluctuate over time, with periods of remission and flare-ups.
How is Inflammatory Bowel Disease diagnosed?
IBD is typically diagnosed through a combination of physical examination, medical history review, and various tests, such as blood tests, stool tests, imaging studies (e.g., X-rays, CT scans, or MRI), and endoscopic procedures (e.g., colonoscopy or sigmoidoscopy). A biopsy of the affected tissue may also be performed during an endoscopic procedure to help confirm the diagnosis.
How can Inflammatory Bowel Disease be treated?
Treatment for IBD focuses on managing symptoms, reducing inflammation, and preventing complications. Common treatments include medications (e.g., anti-inflammatory drugs, immune system suppressors, or antibiotics), dietary modifications, and, in some cases, surgery. The specific treatment plan will depend on the type and severity of the disease, as well as the individual's overall health.
What complications may occur with Inflammatory Bowel Disease?
Complications of IBD can include intestinal blockages, ulcers, fistulas, abscesses, malnutrition, and an increased risk of colon cancer. In some cases, IBD can also cause extra-intestinal manifestations, affecting other organs and systems in the body.
How can I prevent Inflammatory Bowel Disease?
There is no known way to prevent IBD, as the exact cause remains unclear. However, maintaining a healthy lifestyle, including a balanced diet and regular exercise, can help support overall health and may reduce the risk of other chronic conditions.
Long-term management of Inflammatory Bowel Disease
Long-term management of IBD involves regular monitoring by your healthcare team, adherence to medication regimens, and maintaining a healthy lifestyle to minimize the risk of complications. This includes following a well-balanced diet, staying hydrated, exercising regularly, and managing stress. In some cases, individuals may require ongoing medical treatments or surgery.
What is recent research saying about Inflammatory Bowel Disease?
Recent research on IBD has focused on understanding the genetic, environmental, and immune system factors that contribute to the development of the disease, as well as improving treatment options and outcomes. Some studies have explored the role of the gut microbiome in IBD and the potential for using probiotics or fecal microbiota transplantation as a treatment. Additionally, researchers are investigating the effectiveness of new medications, including biologic therapies, and personalized treatment approaches based on the individual's genetic makeup and disease characteristics.
Where can I go for more information on Inflammatory Bowel Disease?
For more information on inflammatory bowel disease, consult your healthcare provider or visit reputable health organizations' websites, such as the Crohn's & Colitis Foundation, the American Gastroenterological Association (AGA), or the US Centers for Disease Control and Prevention (CDC). These organizations provide comprehensive information on IBD, including prevention, treatment, management strategies, and ongoing research.

