Interstitial Cystitis
What is Interstitial Cystitis?
Interstitial cystitis (IC), also known as painful bladder syndrome, is a chronic condition that causes pain, pressure, and discomfort in the bladder and surrounding pelvic region. The condition affects both men and women, although it is more common in women, and can significantly impact a person's quality of life.
Who's at risk for Interstitial Cystitis?
Interstitial cystitis can affect people of all ages, but it is most commonly diagnosed in individuals between the ages of 30 and 50. Women are at a higher risk for developing IC than men. Other risk factors for IC include having a family history of the condition, having another chronic pain disorder (such as fibromyalgia or irritable bowel syndrome), and experiencing physical or emotional trauma.
What causes Interstitial Cystitis?
The exact cause of interstitial cystitis is not well understood, but it is believed to involve a combination of genetic, environmental, and immune system factors. Some researchers theorize that IC may be caused by damage to the bladder lining, an autoimmune reaction, or the release of inflammatory substances in the bladder.
How does Interstitial Cystitis start?
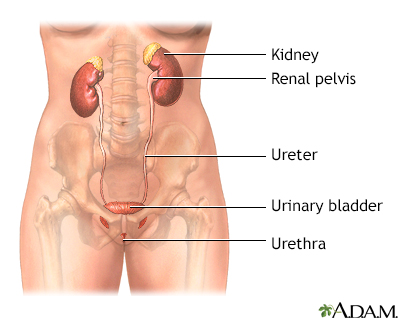
Interstitial cystitis is thought to begin when the protective lining of the bladder becomes damaged or compromised, allowing irritating substances in the urine to penetrate the bladder wall. This damage may trigger an immune response, inflammation, and the development of the chronic pain and discomfort characteristic of IC.
What are the symptoms of Interstitial Cystitis?
The symptoms of interstitial cystitis can vary widely and may include frequent urination, a persistent urge to urinate, bladder pain or pressure, and pain or discomfort in the lower abdomen or pelvic area. The severity and frequency of symptoms can fluctuate over time, with periods of remission and flare-ups. Symptoms may also be influenced by factors such as stress, menstruation, or certain foods and beverages.
How is Interstitial Cystitis diagnosed?
Diagnosing interstitial cystitis can be challenging, as there is no specific test for the condition, and its symptoms can overlap with other urinary disorders. The diagnostic process typically involves a physical examination, a review of your medical history and symptoms, and various tests to rule out other possible causes, such as urinary tract infections, bladder cancer, or kidney stones. These tests may include urinalysis, bladder function tests, cystoscopy, and imaging studies.
How can Interstitial Cystitis be treated?
Treatment for interstitial cystitis focuses on managing symptoms and improving quality of life. There is no one-size-fits-all treatment, and a combination of therapies may be necessary. Common treatments include medications (e.g., oral or bladder-instilled medications to reduce pain and inflammation), physical therapy, stress management techniques, and dietary modifications. In some cases, more invasive procedures, such as nerve stimulation, bladder distention, or surgery, may be considered.
What complications may occur with Interstitial Cystitis?
Interstitial cystitis can lead to several complications, including reduced bladder capacity, chronic pain, sleep disturbances, and emotional distress, such as depression or anxiety. Additionally, IC can have a significant impact on a person's work, social life, and intimate relationships.
How can I prevent Interstitial Cystitis?
There is currently no known way to prevent interstitial cystitis, as the exact cause remains unclear. However, maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can help support overall health and may reduce the risk of other chronic conditions.
Long-term management of Interstitial Cystitis
Long-term management of interstitial cystitis involves working closely with your healthcare team to develop a personalized treatment plan that addresses your specific needs and symptoms. This may include ongoing medical treatments, lifestyle modifications (such as dietary changes and stress management techniques), and regular monitoring to track your progress and adjust your treatment plan as needed. It is also essential to maintain open communication with your healthcare provider and seek support from friends, family, or support groups to help you cope with the challenges of living with IC.
What is recent research saying about Interstitial Cystitis?
Recent research on interstitial cystitis has focused on better understanding the underlying causes of the condition, identifying potential biomarkers for diagnosis, and developing new treatment options. Some studies have explored the role of the bladder's protective lining, the immune system, and the nervous system in the development of IC. Additionally, researchers are investigating potential new medications and therapies, such as targeted drug delivery, stem cell therapy, and nerve modulation, to improve the management of the condition.
Where can I go for more information on Interstitial Cystitis?
For more information on interstitial cystitis, consult your healthcare provider or visit reputable health organizations' websites, such as the Interstitial Cystitis Association (ICA), the American Urological Association (AUA), or the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). These organizations provide comprehensive information on interstitial cystitis, including prevention, treatment, management strategies, and ongoing research.

