Myelofibrosis
What is Myelofibrosis?
Myelofibrosis is a rare bone marrow disorder in which the bone marrow becomes fibrous and scarred, leading to a reduced ability to produce healthy blood cells. This can result in anemia, an enlarged spleen (splenomegaly), and a variety of other symptoms. Myelofibrosis is classified as a type of chronic myeloproliferative neoplasm, a group of disorders characterized by the overproduction of blood cells.
Who's at risk for Myelofibrosis?
Myelofibrosis typically affects older adults, with most cases occurring in individuals over the age of 50. However, it can occur in younger individuals as well. The exact cause of myelofibrosis is unknown, but certain genetic mutations have been identified in many patients with the condition. There is no clear evidence that environmental factors or lifestyle habits significantly influence the risk of developing myelofibrosis.
What causes Myelofibrosis?
The exact cause of myelofibrosis is unknown, but it is believed to involve genetic mutations that affect the normal functioning of hematopoietic stem cells in the bone marrow. These mutations lead to the overproduction of blood cells and the development of fibrous scar tissue in the bone marrow. In some cases, myelofibrosis may evolve from other myeloproliferative neoplasms, such as polycythemia vera or essential thrombocythemia.
How does Myelofibrosis start?
Myelofibrosis starts when genetic mutations disrupt the normal functioning of hematopoietic stem cells in the bone marrow, causing them to produce too many blood cells and prompting the formation of fibrous scar tissue. This scarring impairs the bone marrow's ability to produce healthy blood cells, leading to the various symptoms associated with myelofibrosis.
What are the symptoms of Myelofibrosis?
Symptoms of myelofibrosis can vary widely and may include fatigue, shortness of breath, weakness, easy bruising or bleeding, bone pain, fever, night sweats, and weight loss. An enlarged spleen is a common symptom and can cause abdominal pain or a feeling of fullness. In some cases, myelofibrosis may progress slowly and not cause noticeable symptoms for years.
How is Myelofibrosis diagnosed?
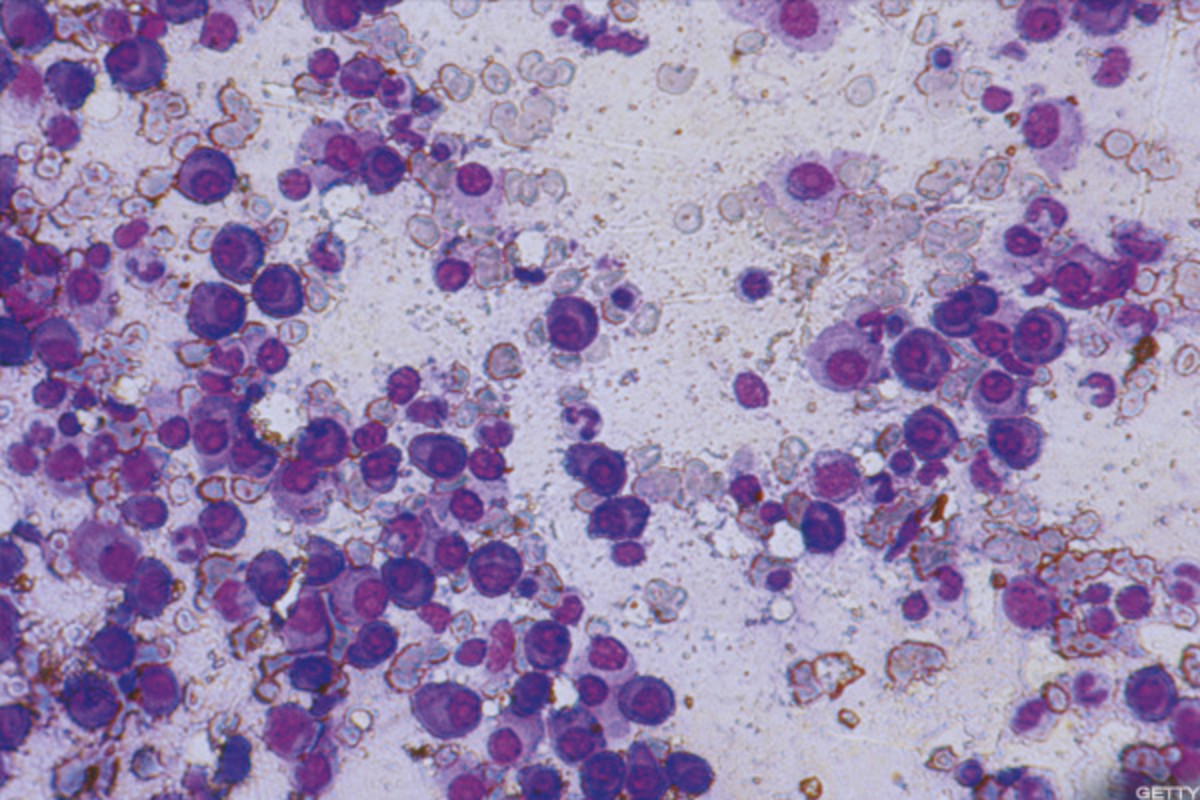
Myelofibrosis is typically diagnosed through a combination of medical history, physical examination, blood tests, and bone marrow biopsy. Blood tests can reveal anemia, abnormal blood cell counts, and the presence of certain genetic mutations. A bone marrow biopsy can confirm the presence of fibrous scar tissue and help to rule out other potential causes of the patient's symptoms.
How can Myelofibrosis be treated?
There is currently no cure for myelofibrosis, but treatments can help manage symptoms and improve quality of life. Treatment options may include blood transfusions, medications to manage anemia or reduce spleen size, chemotherapy, targeted therapies, or immunomodulatory drugs. In some cases, a stem cell transplant may be considered for eligible patients, which has the potential to cure the disease.
What complications may occur with Myelofibrosis?
Complications associated with myelofibrosis can include an increased risk of infections, bleeding or clotting issues, an enlarged spleen, bone pain, and an increased risk of developing acute leukemia. Additionally, the reduced production of healthy blood cells can lead to anemia, which may further contribute to fatigue and other symptoms.
How can I prevent Myelofibrosis?
Since the exact cause of myelofibrosis is unknown and there are no established lifestyle or environmental risk factors, there are no specific prevention measures that can be taken. However, maintaining a healthy lifestyle and staying informed about your family's medical history can help you be more proactive about your overall health. Early detection and proper management of myelofibrosis can help to minimize complications and improve quality of life.
Long-term management of Myelofibrosis
Long-term management of myelofibrosis involves ongoing monitoring of the condition, managing symptoms, and adjusting treatments as needed. Regular follow-up appointments with your healthcare provider are essential to track the progression of the disease and to ensure that any complications are addressed promptly. It is also important to maintain a healthy lifestyle, engage in regular physical activity, and practice stress management techniques to improve overall well-being.
What is recent research saying about Myelofibrosis?
Recent research on myelofibrosis has focused on understanding the genetic factors that contribute to the development of the disease, as well as exploring new treatment options, such as targeted therapies and immunomodulatory drugs. Researchers are also investigating the potential benefits of novel agents, combination therapies, and stem cell transplantation in the treatment of myelofibrosis.
Where can I go for more information on Myelofibrosis?
For more information on myelofibrosis, consult your healthcare provider or visit reputable websites like the Leukemia & Lymphoma Society, the American Cancer Society, or the National Cancer Institute. These organizations provide comprehensive resources on the diagnosis, treatment, and management of myelofibrosis, as well as information on ongoing research and clinical trials.

