Overactive Bladder
What is overactive bladder?
Overactive bladder (OAB) is a condition characterized by a frequent, urgent need to urinate, as well as sometimes experiencing leakage or incontinence. It can have a significant impact on an individual's quality of life, as it may disrupt daily activities and lead to embarrassment or social isolation.
Who's at risk for overactive bladder?
OAB can affect individuals of any age, but it is more common in older adults, particularly women. Other risk factors for OAB may include:
- Certain medical conditions, such as diabetes, obesity, or urinary tract infections
- Certain medications, such as diuretics or muscle relaxants
- Neurological conditions, such as Parkinson's disease or multiple sclerosis
- Previous pelvic surgery or trauma
What causes overactive bladder?
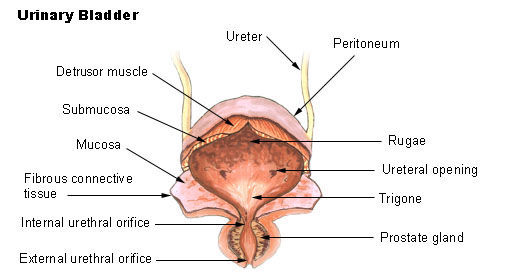
The exact cause of OAB is not well understood, but it is thought to be related to abnormalities in the nerves and muscles of the bladder. These abnormalities may cause the bladder to contract involuntarily, leading to the symptoms of OAB.
How does overactive bladder start?
OAB can start gradually and worsen over time, or it may develop suddenly.
What are the symptoms of overactive bladder?
Symptoms of OAB may include:
- A sudden, urgent need to urinate that is difficult to control
- Frequent urination, often more than eight times per day
- Incontinence or leakage of urine
- Nocturia, or waking up frequently at night to urinate
How is overactive bladder diagnosed?
To diagnose OAB, a healthcare provider may perform a physical exam, take a medical history, and perform certain tests, such as:
- A urine test to check for infection or other abnormalities
- A bladder diary, which involves recording fluid intake, urination frequency, and incontinence episodes over several days
- A post-void residual test to measure how much urine remains in the bladder after urination
- Urodynamic testing, which measures pressure and urine flow in the bladder
How can overactive bladder be treated?
Treatment for OAB may depend on the severity of symptoms and underlying causes. Some common treatments for OAB may include:
- Lifestyle modifications, such as bladder training, timed voiding, and dietary changes
- Medications to relax the bladder muscles or decrease urine production
- Nerve stimulation, such as through sacral neuromodulation or percutaneous tibial nerve stimulation
- Surgery to improve bladder function, such as a bladder augmentation or urinary diversion
What complications may occur with overactive bladder?
OAB can lead to several complications, including:
- Skin irritation or infection due to incontinence or leakage
- Reduced quality of life and social isolation due to embarrassment or inconvenience
- Increased risk of falls or accidents due to urgency or incontinence
How can I prevent overactive bladder?
While there is no surefire way to prevent OAB, some strategies that may help reduce the risk or severity of symptoms include:
- Maintaining a healthy weight
- Staying hydrated and limiting caffeine and alcohol intake
- Practicing good toileting habits, such as fully emptying the bladder during urination
- Performing pelvic floor exercises to strengthen the muscles that support the bladder
Long-term management of overactive bladder
For individuals with OAB, long-term management may be necessary to maintain symptom control and prevent complications. Some strategies for long-term management of OAB may include:
- Regular follow-up appointments with a healthcare provider to monitor symptoms and adjust treatment as necessary
- Continued lifestyle modifications, such as bladder training and pelvic floor exercises
- Regularly taking medications as prescribed by a healthcare provider
- Incorporating strategies to manage incontinence or leakage, such as using absorbent pads or changing clothing as needed
What is recent research saying about overactive bladder?
Recent research has focused on understanding the underlying causes of OAB and developing new treatments. Some areas of research include:
- Investigating the role of the gut microbiome in bladder function and OAB
- Developing new medications that target specific bladder receptors or pathways
- Exploring the use of stem cell therapy to repair damaged bladder tissue
- Studying the effectiveness of behavioral interventions, such as cognitive behavioral therapy, for managing OAB symptoms
Where can I go for more information on overactive bladder?
For more information on OAB, individuals can speak with their healthcare provider or visit reputable websites, such as:

