Pancreatic Cancer
What is pancreatic cancer?
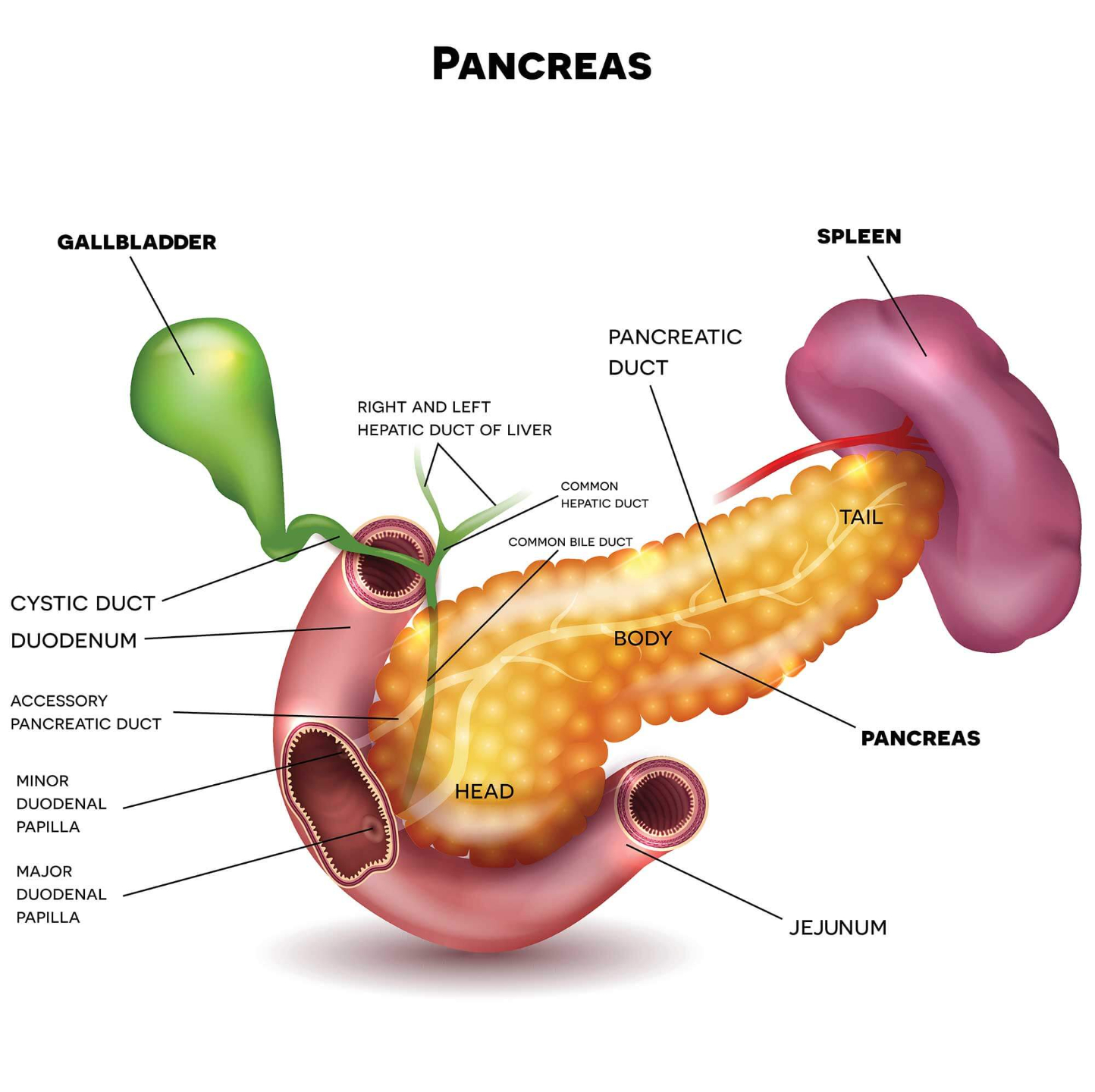
Pancreatic cancer is a type of cancer that arises in the pancreas, an organ located in the abdomen that produces enzymes to aid in digestion and hormones such as insulin to regulate blood sugar levels. It is a serious and often aggressive cancer that can be difficult to diagnose and treat.
Who's at risk for pancreatic cancer?
Pancreatic cancer can occur in individuals of any age, but it is more common in those over the age of 50. Other risk factors include:
- Smoking
- Obesity
- Chronic pancreatitis
- Family history of pancreatic cancer
- Certain genetic mutations, such as BRCA1 and BRCA2
What causes pancreatic cancer?
The exact cause of pancreatic cancer is not fully understood, but it is thought to occur as a result of genetic mutations that lead to uncontrolled cell growth in the pancreas. Risk factors such as smoking, obesity, and chronic pancreatitis may increase the likelihood of developing these mutations.
How does pancreatic cancer start?
Pancreatic cancer typically arises in the cells lining the ducts or small glands within the pancreas. Over time, these cells may begin to grow and divide uncontrollably, forming a tumor that can invade nearby tissues and organs.
What are the symptoms of pancreatic cancer?
Pancreatic cancer may not cause symptoms in its early stages, but as the cancer grows and spreads, it can cause a variety of symptoms, including:
- Abdominal pain or discomfort
- Loss of appetite
- Unexplained weight loss
- Jaundice (yellowing of the skin and eyes)
- Fatigue
- Nausea and vomiting
- New-onset diabetes or changes in blood sugar levels
How is pancreatic cancer diagnosed?
Pancreatic cancer may be diagnosed through a variety of tests and procedures, including:
- Imaging tests such as CT scans, MRI, or ultrasound
- Blood tests to look for markers of pancreatic cancer
- Biopsy, which involves removing a small sample of pancreatic tissue for analysis
How can pancreatic cancer be treated?
Treatment for pancreatic cancer may depend on the stage and location of the cancer, as well as the individual's overall health. Options may include:
- Surgery to remove the tumor or a portion of the pancreas
- Radiation therapy to kill cancer cells
- Chemotherapy to target cancer cells throughout the body
- Targeted therapy, which uses drugs to target specific genes or proteins involved in cancer growth
What complications may occur with pancreatic cancer?
Pancreatic cancer can cause a range of complications, including:
- Obstruction of the bile duct, leading to jaundice and other symptoms
- Spread of cancer to other organs and tissues
- Pancreatic enzyme deficiencies, leading to malabsorption of nutrients
How can I prevent pancreatic cancer?
While there is no sure way to prevent pancreatic cancer, individuals can take steps to reduce their risk, including:
- Quitting smoking
- Maintaining a healthy weight
- Limiting alcohol intake
- Managing diabetes
- Being aware of family history and genetic risk factors
Long-term management of pancreatic cancer
Long-term management of pancreatic cancer may involve ongoing treatment and monitoring to detect any signs of recurrence or spread. Palliative care may also be appropriate to manage symptoms and improve quality of life.
What is recent research saying about pancreatic cancer?
Recent research in pancreatic cancer is focused on improving early detection and developing new treatments to improve outcomes. Other areas of research include:
- Understanding the genetic changes involved in pancreatic cancer
- Developing new immunotherapies to target cancer cells
- Improving the use of existing treatments, such as radiation and chemotherapy
Where can I go for more information on pancreatic cancer?
For more information on pancreatic cancer, individuals can speak with their healthcare provider or visit reputable websites, such as:

