Stiff Person Syndrome
What is Stiff-person Syndrome?
Stiff-person Syndrome (SPS) is a rare neurological disorder characterized by stiffness and functional impairment of the skeletal muscles. The stiffness primarily affects the trunk and lower limbs, often resulting in an abnormal posture and limited mobility. The muscles affected are often in a state of continual contraction, leading to painful spasms triggered by external stimuli or stress.
Who's at Risk for Stiff-person Syndrome?
While SPS can affect people of any age, it most commonly presents in adulthood between the ages of 30 and 50. It is more common in women than men. People with autoimmune conditions, such as type 1 diabetes, thyroiditis, or vitiligo, are at a heightened risk, reflecting the autoimmune nature of SPS.
What Causes Stiff-person Syndrome?
The exact cause of SPS is not fully understood. However, it is believed to be an autoimmune disorder, where the body's immune system mistakenly attacks its own tissues. In this case, it targets the central nervous system, particularly the brain and spinal cord, leading to a reduction in a substance called glutamic acid decarboxylase (GAD), which plays a critical role in controlling muscle movement.
How does Stiff-person Syndrome Start?
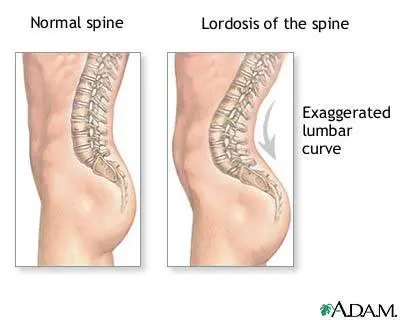
Stiff-person Syndrome typically starts subtly, often with stiffness in the back and legs, and an exaggerated upright posture. It may be mistaken for other conditions, such as Parkinson's disease, multiple sclerosis, or anxiety disorders, in its early stages.
What are the Symptoms of Stiff-person Syndrome?
Symptoms of SPS include stiffness in the muscles of the trunk and limbs, often accompanied by painful muscle spasms. There may be functional impairment and decreased mobility. Symptoms can worsen with stress, sudden movements, or external stimuli like loud noises. Some people may also experience emotional disturbances like depression or anxiety.
How is Stiff-person Syndrome Diagnosed?
Diagnosis of SPS can be challenging due to its rarity and overlapping symptoms with other conditions. It is primarily diagnosed through a combination of clinical symptoms, electromyography (EMG) to assess muscle activity, and blood tests to detect the presence of specific autoantibodies such as anti-GAD antibodies.
How can Stiff-person Syndrome be Treated?
Treatment for SPS is primarily symptomatic and often involves a multidisciplinary approach. This may include medications such as benzodiazepines, baclofen, or immunotherapies to manage symptoms. Physical therapy can also be beneficial in managing stiffness and improving mobility.
What Complications may Occur with Stiff-person Syndrome?
Complications can arise from the muscle stiffness and mobility issues, including falls and related injuries, difficulty walking, and in severe cases, disability. Depression and anxiety can also occur due to the chronic nature of the condition and its impact on quality of life.
How can I Prevent Stiff-person Syndrome?
As the cause of SPS is not entirely understood, there are no definitive preventive measures. However, regular follow-ups with healthcare professionals, especially for those with autoimmune disorders, can help with early detection and management.
Long-term Management of Stiff-person Syndrome
Long-term management of SPS involves regular medication to control symptoms and prevent exacerbations. Regular physiotherapy sessions can also help maintain mobility and function. Psychological support may be necessary to manage associated mental health issues.
What is Recent Research Saying About Stiff-person Syndrome?
Recent research is focused on understanding the autoimmune basis of SPS and exploring new treatment modalities. Studies are being conducted to investigate the role of different autoantibodies and their correlation with disease severity.
Where can I go for more Information on Stiff-person Syndrome?
For more information on Stiff-person Syndrome, you can visit reputable health and medical research websites such as the National Institutes of Health (NIH), Mayo Clinic, and the National Organization for Rare Disorders (NORD). Additionally, reaching out to your healthcare provider or a neurologist can provide more personalized information and guidance.

