Tourette Syndrome
What is Tourette Syndrome?
Tourette syndrome is a neurodevelopmental disorder characterized by involuntary and repetitive movements and vocalizations called tics. These tics can range from mild to severe and may change in frequency and intensity over time. Tourette syndrome typically emerges in childhood or adolescence and often coexists with other conditions such as attention-deficit/hyperactivity disorder (ADHD) or obsessive-compulsive disorder (OCD). Although the exact cause of Tourette syndrome is unknown, it is believed to involve a combination of genetic, environmental, and neurological factors.
Who's at risk for Tourette Syndrome?
Tourette syndrome is estimated to affect around 1% of the population, and it occurs in all ethnic groups. It is more common in males than females, with boys being three to four times more likely to develop the condition. The disorder usually emerges between the ages of 3 and 9, with symptoms peaking in the early teens and often improving or diminishing in adulthood. Having a family history of Tourette syndrome or other tic disorders increases the risk of developing the condition.
What causes Tourette Syndrome?
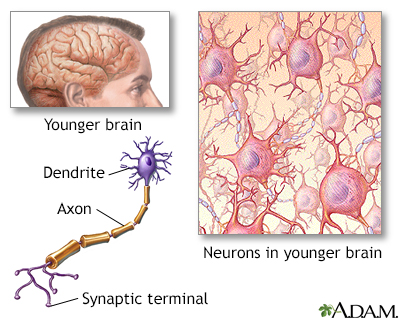
The exact cause of Tourette syndrome is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Genetic studies have identified several genes associated with the disorder, suggesting a genetic predisposition. However, the expression of these genes alone is not sufficient to cause Tourette syndrome, indicating that environmental factors may play a role in triggering the condition. Neurological abnormalities in the brain, such as differences in the structure or function of certain brain regions or neurotransmitter imbalances, may also contribute to the development of Tourette syndrome.
How does Tourette Syndrome start?
Tourette syndrome typically starts in childhood or adolescence, with the onset of tics. The tics can be motor tics, involving movements such as eye blinking, facial grimacing, head jerking, or limb movements, or they can be vocal tics, involving sounds such as throat clearing, grunting, or repetitive speech. The tics may initially be mild and intermittent, but they can increase in frequency and severity over time. Tics often fluctuate in response to various factors, such as stress, excitement, fatigue, or illness.
What are the symptoms of Tourette Syndrome?
The primary symptoms of Tourette syndrome are motor and vocal tics. Motor tics involve sudden, brief, and repetitive movements, while vocal tics involve involuntary sounds or words. Motor tics can range from simple tics, such as eye blinking or shoulder shrugging, to complex tics, such as jumping or touching objects in a particular order. Vocal tics can include throat clearing, grunting, sniffing, or repeating words or phrases. In addition to tics, individuals with Tourette syndrome may experience associated conditions like ADHD, OCD, anxiety, or mood disorders.
How is Tourette Syndrome diagnosed?
Diagnosing Tourette syndrome involves a comprehensive evaluation of symptoms, medical history, and a physical examination. The healthcare provider will assess the presence, frequency, and duration of tics and evaluate any associated conditions. Diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) are used to guide the diagnosis. There is no specific test for Tourette syndrome, but medical tests, such as blood tests or brain imaging, may be conducted to rule out other conditions that could cause similar symptoms.
How can Tourette Syndrome be treated?
While there is no cure for Tourette syndrome, treatment focuses on managing the symptoms and improving overall quality of life. Treatment approaches may include:
- Education and support: Providing information about Tourette syndrome, including understanding and managing symptoms, can help individuals and their families cope with the condition effectively.
- Behavioral therapy: Behavioral therapy, such as cognitive-behavioral therapy (CBT) or habit reversal training (HRT), can help individuals recognize and manage tics, reduce stress, and improve self-control.
- Medications: In some cases, medications may be prescribed to help manage tics or associated conditions. These may include dopamine blockers, alpha-adrenergic agonists, or other medications that target specific symptoms.
- Supportive therapies: Additional therapies, such as occupational therapy or speech therapy, may be beneficial in addressing specific functional difficulties related to Tourette syndrome.
- Management of associated conditions: Treating and managing associated conditions, such as ADHD or OCD, can help improve overall functioning and quality of life.
What complications may occur with Tourette Syndrome?
Tourette syndrome itself is not life-threatening, but it can have a significant impact on daily functioning and quality of life. Complications associated with Tourette syndrome can include:
- Social challenges: Tics can cause embarrassment, social stigma, or difficulties in social interactions, leading to social isolation or low self-esteem.
- Academic or occupational difficulties: Tics and associated conditions may interfere with concentration, attention, or productivity in academic or occupational settings.
- Emotional and psychological impact: Living with Tourette syndrome can lead to emotional distress, anxiety, or depression, particularly when coping with the challenges and societal misconceptions associated with the condition.
How can I prevent Tourette Syndrome?
As the exact cause of Tourette syndrome is unknown, there are no specific preventive measures to avoid its development. However, early detection and appropriate management of symptoms can help minimize the impact of the condition and improve outcomes. Seeking medical attention at the onset of tics or when concerns arise is important to receive a proper diagnosis and establish a suitable treatment plan.
Long-term management of Tourette Syndrome
Long-term management of Tourette syndrome involves an ongoing collaborative approach between the individual, their family, healthcare providers, and educators. It includes consistent monitoring of symptoms, regular follow-up appointments, and adjustments to the treatment plan as needed. Developing coping strategies, stress management techniques, and self-advocacy skills are essential for individuals with Tourette syndrome. Education and awareness initiatives within the community can help reduce stigma and promote understanding of Tourette syndrome.
What is recent research saying about Tourette Syndrome?
Recent research on Tourette syndrome has focused on understanding the underlying neurobiological mechanisms, genetic factors, and exploring potential therapeutic approaches. Advances in neuroimaging techniques have provided insights into the structural and functional brain abnormalities associated with Tourette syndrome. Research on genetic factors aims to identify specific genes involved in the development of the condition. Studies on novel treatments, such as deep brain stimulation or neurofeedback, are exploring their effectiveness in managing severe cases of Tourette syndrome.
Where can I go for more information on Tourette Syndrome?
For more information on Tourette syndrome, reliable sources such as the Tourette Association of America, the National Institute of Neurological Disorders and Stroke (NINDS), or reputable medical centers specializing in neurology or neuropsychiatry can provide valuable information and resources. These organizations offer comprehensive information on Tourette syndrome, including educational materials, support networks, and ongoing research updates. Consulting with a healthcare professional, such as a neurologist or psychiatrist specializing in movement disorders, can also provide personalized information and guidance specific to an individual's situation.

