Toxoplasmosis
What is Toxoplasmosis?
Toxoplasmosis is a parasitic infection caused by the protozoan parasite Toxoplasma gondii. This parasite is found worldwide and can infect humans and other warm-blooded animals. In most healthy individuals, toxoplasmosis causes mild or no symptoms. However, it can be a serious concern for pregnant women, people with weakened immune systems, and individuals with certain pre-existing medical conditions. Toxoplasmosis is primarily acquired through the ingestion of undercooked meat or through contact with cat feces containing the parasite.
Who's at risk for Toxoplasmosis?
While anyone can be at risk for toxoplasmosis, certain groups are more susceptible to severe complications:
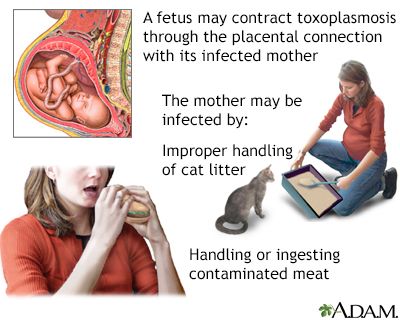
- Pregnant women: Toxoplasmosis can be transmitted from mother to fetus, potentially causing severe congenital complications.
- People with weakened immune systems: Individuals with conditions such as HIV/AIDS, organ transplant recipients, and those undergoing chemotherapy are at a higher risk of developing severe toxoplasmosis due to their compromised immune function.
- Individuals with certain pre-existing medical conditions: People with ocular diseases, such as uveitis, or those with congenital toxoplasmosis may experience more severe symptoms if they become infected or have a reactivation of the parasite.
What causes Toxoplasmosis?
Toxoplasmosis is caused by the Toxoplasma gondii parasite. The parasite has a complex life cycle involving different hosts. Cats are the definitive hosts, where the parasite sexually reproduces. The infection is primarily acquired through:
- Ingesting undercooked or raw meat from infected animals, especially pork, lamb, or venison.
- Ingesting food or water contaminated with oocysts, which are microscopic eggs shed in the feces of infected cats.
- Direct contact with contaminated soil, such as gardening or handling cat litter boxes.
Once inside the body, the parasite invades cells and forms cysts, particularly in the brain, muscles, and eyes, where it can remain for years.
How does Toxoplasmosis start?
Toxoplasmosis typically starts with the ingestion of the Toxoplasma gondii parasite. This can occur by consuming contaminated meat, accidentally ingesting oocysts from cat feces, or through other means of exposure. Once inside the body, the parasite undergoes a series of developmental stages, initially multiplying in the intestines and then spreading to other organs. The immune system usually controls the infection, leading to a latent or chronic phase characterized by the presence of cysts. In individuals with weakened immune systems, the parasite can reactivate, leading to more severe symptoms.
What are the symptoms of Toxoplasmosis?
Many people with Toxoplasma gondii infection do not experience any symptoms or have only mild flu-like symptoms. However, symptoms can vary depending on the individual's immune status and the stage of infection. Common symptoms may include:
- Fatigue
- Fever
- Muscle aches
- Swollen lymph nodes
- Sore throat
- Headache
- Eye redness or blurred vision (ocular toxoplasmosis)
In individuals with weakened immune systems, the infection can cause more severe symptoms, including confusion, seizures, lung problems, or neurological complications.
How is Toxoplasmosis diagnosed?
Toxoplasmosis is diagnosed through a combination of medical history, symptoms, and laboratory tests. A healthcare professional will inquire about potential exposure to the parasite and perform a physical examination. Laboratory tests, including blood tests, can detect the presence of antibodies to Toxoplasma gondii. In some cases, additional tests, such as polymerase chain reaction (PCR) or antibody avidity testing, may be conducted to confirm the diagnosis or assess the timing of the infection.
How can Toxoplasmosis be treated?
In healthy individuals with mild or no symptoms, treatment for toxoplasmosis may not be necessary. However, for pregnant women, people with weakened immune systems, or individuals with severe symptoms, treatment is typically recommended. The primary medications used to treat toxoplasmosis are pyrimethamine and sulfadiazine, often combined with folinic acid (leucovorin). These medications help reduce the parasite's replication and control the infection. Treatment duration and specific medications may vary based on the individual's condition and immune status, and close medical monitoring is necessary.
What complications may occur with Toxoplasmosis?
In healthy individuals, toxoplasmosis typically resolves without complications. However, in certain cases, toxoplasmosis can lead to complications such as:
- Congenital toxoplasmosis: In pregnant women, the infection can be transmitted to the fetus, potentially causing severe congenital complications, including neurological, ocular, or systemic abnormalities.
- Ocular toxoplasmosis: Inflammation of the retina and other eye structures can occur, leading to vision problems or even permanent vision loss.
- Encephalitis: Severe cases of toxoplasmosis can result in brain inflammation (encephalitis), which may cause neurological symptoms, seizures, or cognitive impairments.
- Reactivation in immunocompromised individuals: People with weakened immune systems are at risk of the parasite reactivating, leading to more severe symptoms and potentially life-threatening complications.
How can I prevent Toxoplasmosis?
To reduce the risk of Toxoplasma gondii infection, several preventive measures can be taken:
- Cooking meat thoroughly: Cook meat to safe temperatures to kill any potential parasites. Use a food thermometer to ensure proper cooking.
- Practicing good hygiene: Wash hands thoroughly with soap and water after handling raw meat, gardening, or handling cat litter boxes. Clean cooking utensils and surfaces properly.
- Avoiding consumption of raw or undercooked meat: Avoid eating raw or undercooked meat, particularly pork, lamb, or venison.
- Safe food handling: Prevent cross-contamination by keeping raw and cooked foods separate. Use separate cutting boards and utensils for raw and cooked foods.
- Preventing contact with cat feces: Wear gloves while gardening, and wash hands thoroughly afterward. Pregnant women should avoid handling cat litter boxes and have someone else do it.
- Avoiding contaminated water and soil: When traveling or engaging in outdoor activities, be cautious about consuming untreated water and coming into contact with potentially contaminated soil.
- Ensuring proper cat care: Keep cats indoors to prevent them from hunting and becoming infected. Feed cats commercial cat food to minimize their exposure to potential sources of infection.
Long-term management of Toxoplasmosis
Long-term management of toxoplasmosis varies depending on the individual's specific circumstances. Pregnant women and individuals with weakened immune systems require close medical monitoring and follow-up care. Prevention of future infections and minimizing the risk of complications are important considerations. Regular check-ups, appropriate medications (if necessary), and adherence to preventive measures can help manage the condition effectively.
What is recent research saying about Toxoplasmosis?
Recent research on toxoplasmosis has focused on various aspects, including understanding the parasite's biology, developing improved diagnostic techniques, and investigating potential treatment options. Studies have explored the impact of toxoplasmosis on mental health and neurologic conditions. Additionally, research continues to explore the development of vaccines and new medications to improve treatment outcomes.
Where can I go for more information on Toxoplasmosis?
For more information on toxoplasmosis, reliable sources such as the Centers for Disease Control and Prevention (CDC), the National Institutes of Health (NIH), or reputable infectious disease organizations can provide valuable information and resources. These organizations offer comprehensive information on toxoplasmosis, including prevention strategies, treatment guidelines, and the latest research updates. Consulting with a healthcare professional, such as an infectious disease specialist or obstetrician, can also provide personalized information and guidance specific to an individual's situation.

