Vasectomy
What is a Vasectomy?
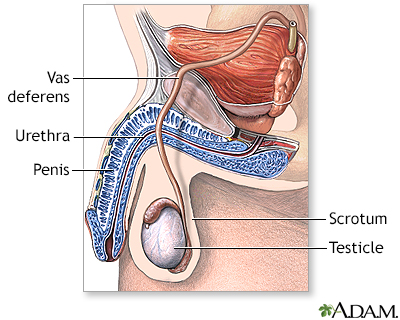
Vasectomy is a surgical procedure performed on males as a method of permanent contraception. It involves cutting or blocking the vas deferens, the tubes that carry sperm from the testicles to the urethra. By interrupting the flow of sperm, a vasectomy prevents sperm from reaching the semen ejaculated during sexual intercourse, thereby making a person sterile and unable to father children.
Who's a candidate for a Vasectomy?
Vasectomy is an option for males who are certain they no longer want to father children or who do not desire any future pregnancies. It is generally considered a permanent form of contraception and should only be pursued by individuals who are confident in their decision. It is important for candidates to fully understand the implications and irreversible nature of the procedure.
What does Vasectomy achieve?
Vasectomy is not a result of an underlying medical condition. Instead, it is a deliberate surgical intervention performed by choice to achieve permanent contraception. The procedure intentionally disrupts the vas deferens, preventing the passage of sperm during ejaculation.
What is the procedure for a Vasectomy?
Vasectomy starts with a surgical procedure performed by a healthcare professional, typically a urologist or a specialized surgeon. The procedure may be done in an outpatient setting using local anesthesia. It typically involves the following steps:
- Administration of anesthesia: The scrotum is numbed using a local anesthetic to minimize discomfort during the procedure.
- Access to the vas deferens: The surgeon makes one or two small incisions in the scrotum to access the vas deferens.
- Cutting or blocking the vas deferens: The vas deferens is either cut and a section removed or blocked using techniques like clips, ties, or cauterization.
- Closure of the incisions: The incisions in the scrotum are closed with dissolvable stitches or surgical glue.
- Recovery: Following the procedure, a supportive dressing or scrotal support may be provided to minimize swelling and discomfort.
How might I feel after a Vasectomy?
Vasectomy itself does not typically cause noticeable symptoms. However, immediately following the procedure, individuals may experience some mild discomfort, swelling, or bruising in the scrotal area. These symptoms are usually temporary and can be managed with over-the-counter pain medications and the application of ice packs.
What healthcare professional should I speak to regarding a Vasectomy?
Vasectomy is not diagnosed but rather performed as a deliberate surgical procedure. Before undergoing a vasectomy, individuals should have a detailed discussion with a healthcare professional, such as a urologist, who will explain the procedure, its implications, and answer any questions or concerns. The healthcare professional will also ensure that the individual meets the criteria for the procedure and provide appropriate counseling.
How does the Vasectomy affect fertility?
Vasectomy is the treatment itself, as it is a surgical procedure performed to achieve permanent contraception. The procedure effectively sterilizes a person by blocking or cutting the vas deferens, preventing sperm from mixing with semen during ejaculation. Once the vas deferens is interrupted, the individual can engage in sexual activity without the risk of causing pregnancy.
What complications may occur with Vasectomy?
Vasectomy is generally a safe and effective procedure, but complications can occur, although they are relatively rare. Potential complications may include:
- Bleeding or hematoma: Some individuals may experience bleeding or the formation of a blood clot (hematoma) in the scrotal area following the procedure.
- Infection: Although uncommon, infections can occur at the incision sites or in the scrotal area.
- Chronic pain: Some individuals may experience chronic pain in the scrotal area, known as post-vasectomy pain syndrome. This is a rare complication.
- Recanalization: In very rare cases, the vas deferens can spontaneously reconnect, leading to the restoration of sperm flow and the potential for pregnancy. This is why it is important to confirm the success of the procedure through post-vasectomy semen analysis.
- Emotional considerations: It is important to carefully consider the irreversible nature of the procedure and potential emotional implications, especially for individuals who may later desire children or experience changes in their personal circumstances.
How can I reverse a Vasectomy?
If an individual is considering a vasectomy but wants to maintain the potential for future fertility, it is recommended to explore alternative contraception methods or consider other options such as sperm banking.
It is possible to attempt a reversal of a vasectomy through a surgical procedure known as vasectomy reversal or vasovasostomy. Vasectomy reversal reconnects the severed ends of the vas deferens, allowing the flow of sperm to be restored. However, it's important to note that the success of vasectomy reversal depends on various factors, including the length of time since the vasectomy, the technique used during the initial procedure, and individual factors such as age and fertility status.
Vasectomy reversal is a more complex and delicate surgery compared to vasectomy. It typically requires specialized surgical techniques and is performed by a skilled urologist or microsurgeon. The success rates of vasectomy reversal can vary, with factors such as the presence of sperm antibodies, scar tissue, or the development of blockages affecting the outcome.
It's essential to have a consultation with a urologist or a specialist in reproductive medicine to assess the potential for successful reversal based on individual circumstances. They can provide a comprehensive evaluation, discuss the available options, and guide you through the decision-making process.
Alternatively, if vasectomy reversal is not successful or not desired, other options for achieving pregnancy may include assisted reproductive technologies such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). These methods involve retrieving sperm directly from the testicles or using donor sperm to fertilize eggs.
It's crucial to have open and honest discussions with healthcare professionals specializing in fertility and reproductive medicine to explore the most suitable options based on individual circumstances and goals.
Where can I go for more information on Vasectomy?
For more information on vasectomy, reliable sources such as the American Urological Association (AUA), Planned Parenthood, the Mayo Clinic, or other reputable urology organizations and healthcare institutions can provide valuable information and resources. Consulting with a healthcare professional, such as a urologist or primary care physician, can also provide personalized information and guidance specific to an individual's situation.

