Vulvodynia
What is Vulvodynia?
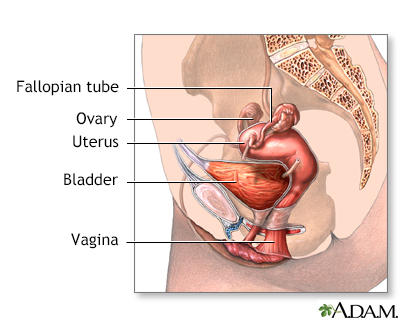
Vulvodynia is a chronic pain condition characterized by persistent discomfort or pain in the vulva, the external genital area in women. The pain may be described as burning, stinging, rawness, or irritation, and it can significantly impact a woman's quality of life, including her sexual function and emotional well-being. Vulvodynia is not associated with any visible signs of inflammation or infection, making it a challenging condition to diagnose and manage.
Who's at risk for Vulvodynia?
Vulvodynia can affect women of all ages, but certain factors may increase the risk of developing the condition, including:
- Age: Vulvodynia can occur at any age, but it often starts in young adulthood.
- History of chronic pain: Individuals with a history of other chronic pain conditions, such as fibromyalgia or irritable bowel syndrome, may be at a higher risk.
- Previous vaginal infections or injuries: Women who have had recurrent vaginal infections, such as yeast infections or urinary tract infections, or have experienced vaginal injuries, such as childbirth trauma or surgical procedures, may be more susceptible.
- Hormonal factors: Fluctuations in hormone levels, such as those occurring during menopause or after childbirth, may contribute to the development of vulvodynia.
- Genetic factors: There may be a genetic predisposition to developing vulvodynia, as the condition can sometimes run in families.
What causes Vulvodynia?
The exact cause of vulvodynia is not fully understood, and multiple factors may contribute to its development. Potential causes and contributing factors include:
- Nerve dysfunction: Abnormal nerve signals or heightened sensitivity in the vulvar area may play a role in the development of vulvodynia.
- Muscle abnormalities: Dysfunction or tension in the pelvic floor muscles may contribute to vulvar pain.
- Hormonal changes: Fluctuations in hormone levels, particularly estrogen, can impact the health and sensitivity of vulvar tissues.
- Inflammation: Some researchers believe that inflammation in the vulvar tissues may contribute to the development of vulvodynia.
- Genetic factors: Certain genetic variations or predispositions may increase the likelihood of developing vulvodynia.
- Trauma or injury: Previous trauma or injury to the vulvar area, such as childbirth, surgery, or recurrent infections, may trigger or worsen vulvodynia in some cases.
- Central sensitization: Some individuals with vulvodynia may have an increased sensitivity to pain due to changes in the way the central nervous system processes pain signals.
It's important to note that vulvodynia is not caused by infection, sexually transmitted diseases, or cancer.
How does Vulvodynia start?
Vulvodynia can start suddenly or gradually, and the onset may be associated with certain triggers or events, such as a yeast infection, injury, or hormonal changes. For some women, vulvar pain may be present constantly, while for others, it may come and go or be triggered by specific activities, such as sexual intercourse or prolonged sitting.
What are the symptoms of Vulvodynia?
The main symptom of vulvodynia is persistent vulvar pain or discomfort. The pain may be described as burning, stinging, rawness, or irritation. Other symptoms that may accompany vulvodynia include:
- Pain during sexual intercourse (dyspareunia)
- Painful tampon insertion
- Pain or discomfort when sitting for long periods (sitting intolerance)
- Irritation or pain from tight clothing or underwear
- Increased sensitivity to touch or pressure in the vulvar area
- Raw or sore feeling in the vulva
- Itching or a sensation of swelling, despite no visible signs of inflammation
Symptoms can vary in severity and may fluctuate over time.
How is Vulvodynia diagnosed?
Diagnosing vulvodynia can be challenging, as there are no specific tests or visible signs to confirm the condition. A healthcare professional, typically a gynecologist or dermatologist specializing in vulvar disorders, will perform a thorough evaluation based on symptoms, medical history, and physical examination. The diagnosis usually involves ruling out other possible causes of vulvar pain, such as infections, skin conditions, or hormonal imbalances. In some cases, additional tests or procedures may be done, such as:
- Pelvic examination: A visual examination of the vulva and vagina to check for any visible signs of inflammation, irritation, or abnormalities.
- Cotton swab test: The healthcare professional may gently touch specific areas of the vulva with a cotton swab to assess pain sensitivity or provoke pain.
- Vaginal pH testing: Testing the pH level of the vagina to rule out infections or imbalances in vaginal flora.
- Cultures or swabs: Collecting samples from the vulva or vagina to test for infections, such as yeast or bacterial vaginosis.
The diagnosis of vulvodynia is primarily based on a combination of symptoms, medical history, and ruling out other possible causes of vulvar pain.
How can Vulvodynia be treated?
The treatment of vulvodynia focuses on managing symptoms and providing relief. Since the condition varies from person to person, a tailored approach is necessary. Treatment options may include:
- Topical medications: The application of topical creams or ointments, such as lidocaine or estrogen creams, to the vulvar area can help reduce pain and discomfort.
- Nerve blocks: In some cases, local anesthetic injections may be administered to help temporarily block pain signals.
- Pelvic floor physical therapy: Working with a specialized physical therapist can help address muscle tension or dysfunction in the pelvic floor, providing relief from vulvar pain.
- Medications: Oral medications, such as tricyclic antidepressants, anticonvulsants, or certain nerve pain medications, may be prescribed to help manage chronic pain associated with vulvodynia.
- Counseling or therapy: In situations where vulvodynia has a significant impact on emotional well-being, counseling or therapy may be beneficial to address the psychological aspects and provide coping strategies.
- Lifestyle modifications: Making certain lifestyle changes can help manage vulvodynia symptoms. These may include avoiding irritants or allergens, wearing loose-fitting clothing, practicing good vulvar hygiene, and using hypoallergenic or unscented products.
The treatment plan should be individualized and may involve a combination of approaches. It's important to work closely with a healthcare professional specializing in vulvar disorders to determine the most appropriate treatment options.
What complications may occur with Vulvodynia?
Vulvodynia can have significant physical, sexual, and emotional impacts on a woman's life. It can affect sexual function, strain intimate relationships, and lead to emotional distress, anxiety, or depression. Chronic pain and discomfort may also disrupt daily activities and quality of life. Seeking support from healthcare professionals, support groups, or counseling services can help address any complications or challenges associated with vulvodynia.
How can I manage Vulvodynia in the long term?
Managing vulvodynia in the long term involves a combination of treatment strategies, self-care, and self-management. Some strategies that may help in the long-term management of vulvodynia include:
- Self-care and vulvar hygiene: Practicing good vulvar hygiene using mild, unscented cleansers and avoiding irritants or allergens can help manage symptoms.
- Avoiding triggers: Identifying and avoiding triggers that worsen symptoms, such as certain fabrics, tight clothing, or specific activities, can be helpful.
- Stress management: Managing stress levels through relaxation techniques, mindfulness, or stress-reducing activities can help reduce symptom flare-ups.
- Sexual well-being: Open communication with intimate partners, exploring alternative sexual activities or positions, and using water-based lubricants can help maintain sexual intimacy while minimizing discomfort.
- Support networks: Seeking support from healthcare professionals, support groups, or online communities can provide valuable guidance, empathy, and information.
It's important to remember that managing vulvodynia may require trial and error to find the most effective combination of strategies. Regular follow-up appointments with a healthcare professional specializing in vulvar disorders are crucial to monitor progress, adjust treatment plans as needed, and address any concerns.
What is recent research saying about Vulvodynia?
Ongoing research on vulvodynia aims to improve our understanding of the condition, identify potential causes, and develop more effective treatment options. Some areas of research include:
- Central sensitization: Investigating the role of central sensitization, where the central nervous system becomes overly responsive to pain signals, in vulvodynia and exploring treatments targeting this mechanism.
- Hormonal factors: Further understanding the impact of hormonal changes, such as menopause or hormonal therapies, on vulvodynia and developing targeted interventions.
- Genetic and immune factors: Investigating genetic and immune system variations associated with vulvodynia to identify potential biomarkers or treatment targets.
- Psychological aspects: Researching the psychological aspects of vulvodynia, such as the impact on mental health and the effectiveness of psychological interventions in managing symptoms.
Where can I go for more information on Vulvodynia?
For more information on vulvodynia, reliable sources such as the International Society for the Study of Vulvovaginal Disease (ISSVD), the National Vulvodynia Association (NVA), or reputable gynecology and dermatology organizations can provide valuable information and resources. Consulting with a healthcare professional specializing in vulvar disorders or seeking referral to a vulvar pain specialist can also provide personalized information and guidance specific to an individual's situation.

