Vulvovaginitis
What is Vulvovaginitis?
Vulvovaginitis is an inflammation or irritation of the vulva and vagina, commonly referred to as the external and internal genital area in women. It is a common condition that can occur at any age, from childhood to adulthood. Vulvovaginitis is often caused by an infection, but it can also be triggered by non-infectious factors such as irritants or allergies.
What causes Vulvovaginitis?
Vulvovaginitis can be caused by various factors, including:
-
Infections:
- Bacterial vaginosis: An overgrowth of certain bacteria in the vagina.
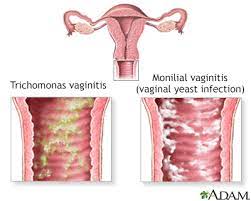
- Yeast infection (vaginal candidiasis): Overgrowth of the Candida fungus in the vagina.
- Trichomoniasis: A sexually transmitted infection caused by the parasite Trichomonas vaginalis.
- Sexually transmitted infections (STIs): Infections such as chlamydia, gonorrhea, or herpes simplex virus can cause vulvovaginitis.
-
Non-infectious causes:
- Irritants: Certain substances, such as perfumed soaps, bubble baths, douches, or scented pads, can irritate the vulva and vagina.
- Allergies: Some women may be allergic to certain products, such as latex condoms or spermicides, leading to vulvovaginal inflammation.
- Hormonal changes: Fluctuations in hormone levels, such as during pregnancy or menopause, can contribute to vulvovaginal irritation.
Who's at risk for Vulvovaginitis?
Vulvovaginitis can affect women of all ages, but certain factors may increase the risk, including:
- Poor hygiene: Inadequate or improper hygiene practices can increase the risk of developing vulvovaginitis.
- Antibiotic use: Taking antibiotics can disrupt the balance of bacteria in the vagina, increasing the risk of infections like yeast infections.
- Sexual activity: Having multiple sexual partners or engaging in unprotected sex can increase the risk of contracting STIs that can cause vulvovaginitis.
- Diabetes: Women with uncontrolled diabetes may be more prone to yeast infections and other vaginal infections.
- Weakened immune system: Conditions that weaken the immune system, such as HIV/AIDS or certain medications, can increase the risk of infections.
How does Vulvovaginitis start?
Vulvovaginitis can start with symptoms such as itching, redness, swelling, or a burning sensation in the vulvar or vaginal area. Discomfort or pain during sexual intercourse or urination may also be present. The onset can be sudden or gradual, depending on the underlying cause.
What are the symptoms of Vulvovaginitis?
The symptoms of vulvovaginitis can vary depending on the cause, but common symptoms may include:
- Itching and irritation of the vulva and vagina
- Redness and swelling of the vulvar area
- Abnormal vaginal discharge, which may be thick, white, yellow, or grayish in color
- Unpleasant odor from the vaginal discharge
- Pain or discomfort during sexual intercourse (dyspareunia)
- Painful or frequent urination
- Vaginal bleeding (less common)
It's important to note that the specific symptoms can vary depending on the cause and individual factors.
How is Vulvovaginitis diagnosed?
To diagnose vulvovaginitis, a healthcare professional, usually a gynecologist or primary care physician, will take a detailed medical history and perform a physical examination. The examination may include a visual inspection of the vulva and vagina, and sometimes a sample of vaginal discharge may be collected for laboratory testing. This can help determine the cause of the vulvovaginitis, whether it's due to an infection or other factors.
In some cases, additional tests may be performed, such as a vaginal pH test, a wet mount microscopy, or cultures, to identify specific pathogens or assess the vaginal environment.
How can Vulvovaginitis be treated?
The treatment of vulvovaginitis depends on the underlying cause. Treatment options may include:
-
Infections:
- Bacterial vaginosis: Antibiotics, such as metronidazole or clindamycin, may be prescribed.
- Yeast infection: Antifungal medications, such as clotrimazole, miconazole, or fluconazole, can be used in the form of creams, suppositories, or oral tablets.
- Trichomoniasis: Prescription medications, such as metronidazole or tinidazole, are commonly used.
- Sexually transmitted infections: Treatment varies depending on the specific infection and may involve antibiotics or antiviral medications.
-
Non-infectious causes:
- Irritants or allergens: Avoiding the use of irritants or allergenic products and practicing good hygiene can help alleviate symptoms.
- Hormonal changes: In some cases, hormonal treatments or moisturizers may be recommended.
It's important to follow the healthcare professional's instructions and complete the prescribed treatment course, even if symptoms improve.
What complications may occur with Vulvovaginitis?
When promptly diagnosed and treated, most cases of vulvovaginitis resolve without complications. However, if left untreated or improperly managed, vulvovaginitis can lead to recurrent infections, chronic inflammation, or the spread of infection to other parts of the reproductive system. Persistent or recurrent vulvovaginal symptoms should be evaluated by a healthcare professional to prevent potential complications.
How can I prevent Vulvovaginitis?
To help prevent vulvovaginitis, consider the following preventive measures:
- Practice good hygiene: Keep the vulva clean and dry, and avoid using harsh soaps or douches. Use mild, fragrance-free products when washing the genital area.
- Wipe from front to back: After using the toilet, always wipe from front to back to prevent the spread of bacteria from the anus to the vaginal area.
- Avoid irritants: Use unscented and hypoallergenic products, such as soaps, detergents, or toilet paper. Avoid tight-fitting clothing or synthetic fabrics that can trap moisture and irritate the vulva.
- Practice safe sex: Use condoms and practice safe sex to reduce the risk of sexually transmitted infections.
- Maintain a healthy lifestyle: Eat a balanced diet, maintain a healthy weight, and manage chronic conditions such as diabetes to reduce the risk of vulvovaginal infections.
Long-term management of Vulvovaginitis
To prevent recurrence or manage chronic vulvovaginitis, it may be helpful to:
- Avoid triggers: Identify and avoid any potential triggers or irritants that may lead to vulvovaginal symptoms.
- Practice self-care: Practice good hygiene, wear breathable cotton underwear, and change out of wet clothing promptly.
- Regular check-ups: Attend regular gynecological check-ups and screenings to detect any potential issues early on.
- Communicate with healthcare professionals: Maintain open communication with healthcare professionals to address any concerns or recurring symptoms.
It's essential to seek medical advice from a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Where can I go for more information on Vulvovaginitis?
For more information on vulvovaginitis, reputable sources such as the American College of Obstetricians and Gynecologists (ACOG), the Centers for Disease Control and Prevention (CDC), the Mayo Clinic, or other trusted gynecology resources can provide valuable information and resources. Consulting with a healthcare professional, such as a gynecologist or primary care physician, can also provide personalized information and guidance specific to an individual's situation.

