Yersinia Pestis
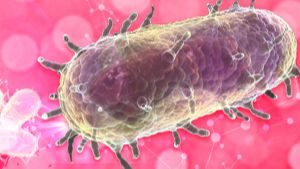
What is Yersinia pestis?
Yersinia pestis is a bacterium responsible for causing the disease known as plague. Plague is an infectious disease that primarily affects rodents and is transmitted to humans through fleas. It is categorized into three forms: bubonic, septicemic, and pneumonic. Yersinia pestis has been responsible for several devastating pandemics throughout history, including the infamous Black Death pandemic in the 14th century.
Who's at risk for Yersinia pestis?
While anyone can be at risk of contracting Yersinia pestis, certain groups may be more susceptible or vulnerable to infection. These include:
- Individuals living in or visiting areas with known plague activity: Plague is endemic in certain regions, particularly in parts of Africa, Asia, and South America. Travelers to these areas may face a higher risk of exposure.
- People with occupational exposure: Individuals who work in occupations with a higher likelihood of contact with rodents, fleas, or other potential carriers of Yersinia pestis, such as hunters, campers, or wildlife workers, may be at an increased risk.
- Individuals with weakened immune systems: People with compromised immune systems, such as those with HIV/AIDS or undergoing immunosuppressive treatments, may be more susceptible to severe infections if exposed to Yersinia pestis.
What causes Yersinia pestis?
Yersinia pestis is primarily transmitted through fleas that infest rodents, particularly rats. Fleas become infected with the bacteria when they feed on the blood of infected rodents. When an infected flea bites a human, it can transmit the bacteria, leading to infection. In rare cases, direct contact with bodily fluids or tissues of infected animals, such as through handling or consuming infected meat, can also result in infection.
How does Yersinia pestis start?
Yersinia pestis infection in humans typically begins when a person is bitten by an infected flea. The bacteria enter the body through the bite wound and multiply in the lymph nodes nearest to the site of entry. From there, the bacteria can spread to other organs and tissues, leading to the manifestation of plague symptoms.
What are the symptoms of Yersinia pestis?
The symptoms of Yersinia pestis infection depend on the form of plague:
- Bubonic plague: The most common form of plague, characterized by the sudden onset of symptoms including fever, chills, headache, fatigue, muscle aches, and swollen and painful lymph nodes (buboes). Buboes typically occur in the groin, armpit, or neck.
- Septicemic plague: This form occurs when the bacteria enter the bloodstream, leading to symptoms such as fever, chills, weakness, abdominal pain, shock, and potentially tissue death (necrosis) in the extremities.
- Pneumonic plague: The most severe and contagious form of plague, characterized by symptoms including high fever, cough, chest pain, difficulty breathing, and bloody or watery sputum.
Pneumonic plague can be transmitted from person to person through respiratory droplets, making it highly dangerous and capable of causing widespread outbreaks if not contained promptly.
How is Yersinia pestis diagnosed?
Diagnosing Yersinia pestis infection involves a combination of clinical evaluation, medical history, and laboratory tests. A healthcare professional may:
- Inquire about symptoms and potential exposure: They will ask about the individual's symptoms, recent travel history, occupation, and possible contact with rodents or fleas.
- Perform a physical examination: The healthcare professional may examine the individual's lymph nodes for signs of swelling or tenderness.
- Conduct laboratory tests: These may include blood tests, such as polymerase chain reaction (PCR) or enzyme-linked immunosorbent assay (ELISA), to detect the presence of Yersinia pestis antigens or antibodies. Blood cultures or other tests may also be performed to isolate and identify the bacteria.
How can Yersinia pestis be treated?
Prompt treatment is essential in managing Yersinia pestis infection. Treatment typically involves the use of antibiotics effective against Yersinia pestis, such as streptomycin, gentamicin, or doxycycline. Treatment duration and specific medications may vary depending on the form and severity of the infection. In severe cases, hospitalization may be necessary for close monitoring and supportive care, including intravenous fluids and other measures to manage complications.
What complications may occur with Yersinia pestis?
Without timely and appropriate treatment, Yersinia pestis infection can lead to severe complications and, in some cases, be fatal. Complications may include:
- Septicemia: The infection can spread throughout the bloodstream, leading to systemic infection and potentially resulting in organ failure, shock, and tissue death.
- Pneumonia and respiratory failure: Pneumonic plague, if left untreated, can cause severe pneumonia and respiratory distress, which may be life-threatening.
- Gangrene and tissue necrosis: In severe cases, inadequate blood supply to tissues can result in gangrene, a condition where tissue dies due to the lack of oxygen and nutrients.
Prevention and early treatment are crucial in minimizing the risk of complications associated with Yersinia pestis infection.
How can I prevent Yersinia pestis?
Preventing Yersinia pestis infection involves various strategies:
- Avoiding exposure to rodents and fleas: Minimize contact with rodents, their nests, and areas where fleas are likely to be present. Implement measures to prevent rodents from entering homes and buildings.
- Using insect repellents: When in areas where plague is endemic or during outbreaks, apply insect repellents to exposed skin and clothing to reduce the risk of flea bites.
- Wearing protective clothing: When spending time outdoors in endemic areas, wear long sleeves, long pants, socks, and closed-toe shoes to reduce the likelihood of flea bites.
- Vaccination: A plague vaccine exists but is generally reserved for individuals at high risk of exposure, such as laboratory workers or those traveling to areas with ongoing outbreaks.
Long-term management of Yersinia pestis
After recovering from Yersinia pestis infection, individuals typically develop immunity to subsequent infections. However, continued preventive measures and surveillance are crucial, particularly in endemic areas or during outbreaks, to minimize the risk of transmission and prevent the resurgence of the disease.
What is recent research saying about Yersinia pestis?
Ongoing research on Yersinia pestis focuses on various aspects, including understanding the genetics and evolution of the bacteria, studying the host-pathogen interactions, improving diagnostic techniques, and exploring potential vaccine candidates. Additionally, research is conducted to monitor and track the presence and distribution of Yersinia pestis in endemic areas to inform public health interventions and response strategies.
Where can I go for more information on Yersinia pestis?
For more information on Yersinia pestis and plague, it is recommended to consult reputable sources such as the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), or local health authorities. These organizations provide up-to-date information on Yersinia pestis, including prevention strategies, treatment guidelines, and the latest research findings.

